The advent of technology has revolutionized numerous sectors, and healthcare is no exception. Virtual Health Assistants (VHAs) have emerged as a significant innovation, leveraging artificial intelligence (AI) and machine learning to enhance patient care and streamline healthcare processes. These digital entities are designed to assist patients in managing their health, providing information, and facilitating communication with healthcare providers.
By integrating VHAs into the healthcare ecosystem, providers can offer more personalized care while improving efficiency and accessibility. VHAs can take various forms, from chatbots that answer patient queries to sophisticated applications that monitor health metrics in real-time. They are increasingly being utilized in telemedicine, chronic disease management, and preventive care, making healthcare more accessible to a broader audience.
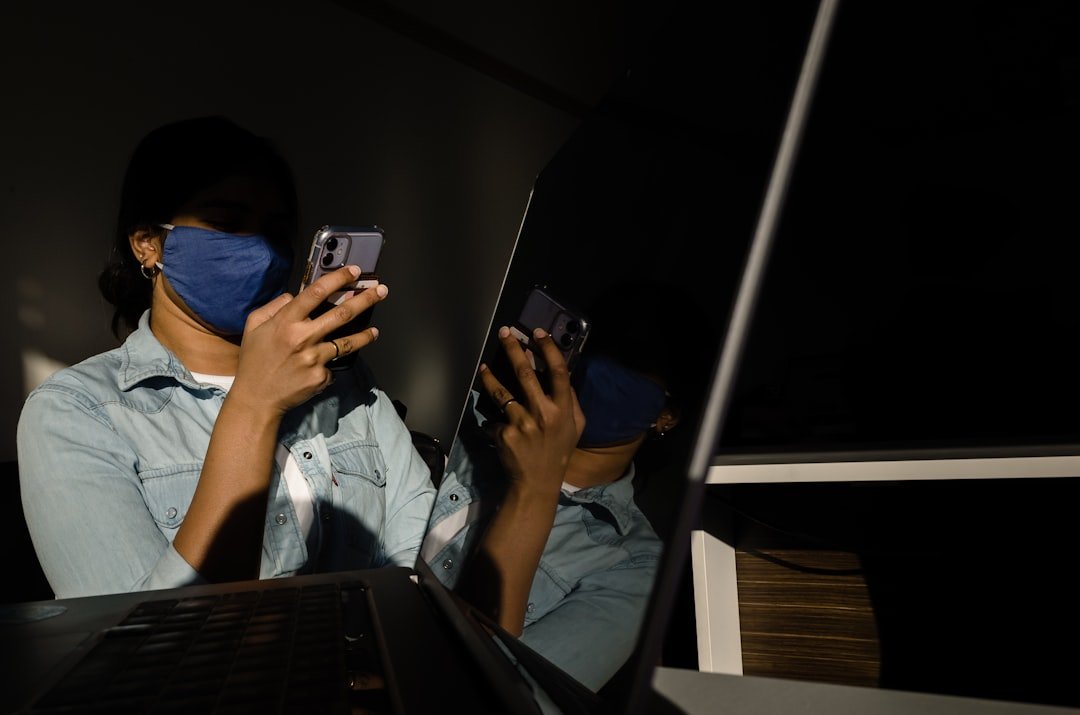
As the demand for remote healthcare solutions continues to grow, particularly in the wake of the COVID-19 pandemic, the role of VHAs is becoming increasingly critical in ensuring that patients receive timely and effective care.
Key Takeaways
- Virtual Health Assistants (VHAs) are digital tools designed to provide support and assistance to patients and healthcare providers in various healthcare settings.
- VHAs offer benefits such as real-time patient monitoring, timely intervention, and improved patient engagement, leading to better health outcomes and reduced healthcare costs.
- VHAs work by using artificial intelligence and machine learning algorithms to analyze patient data, provide personalized recommendations, and communicate with patients through voice or text interfaces.
- Features and capabilities of VHAs include remote monitoring of vital signs, medication reminders, symptom tracking, and personalized health education and coaching.
- VHAs play a crucial role in remote patient monitoring, especially for patients with chronic diseases, by enabling continuous monitoring, early detection of complications, and proactive management of health conditions.
Benefits of Virtual Health Assistants for Patient Monitoring
One of the most significant advantages of Virtual Health Assistants is their ability to facilitate continuous patient monitoring. Unlike traditional methods that often rely on periodic check-ups, VHAs can provide real-time data collection and analysis, allowing healthcare providers to track patients’ health status more effectively. This continuous monitoring is particularly beneficial for patients with chronic conditions such as diabetes or hypertension, where fluctuations in health metrics can have immediate implications for treatment.
Moreover, VHAs can enhance patient engagement by providing personalized feedback and reminders tailored to individual health needs. For instance, a VHA can send medication reminders or dietary suggestions based on a patient’s specific health profile. This proactive approach not only helps patients adhere to their treatment plans but also empowers them to take an active role in managing their health.
The result is a more informed patient population that is better equipped to make decisions about their care.
How Virtual Health Assistants Work
Virtual Health Assistants operate through a combination of natural language processing (NLP), machine learning algorithms, and data analytics. At their core, these systems are designed to understand and respond to user inputs in a conversational manner. When a patient interacts with a VHA, whether through text or voice commands, the system processes the input using NLP techniques to interpret the user’s intent and context.
Once the input is understood, the VHA retrieves relevant information from its database or connects with other healthcare systems to provide accurate responses. For example, if a patient asks about potential side effects of a medication, the VHA can access a comprehensive database of drug information to deliver an informed answer. Additionally, VHAs can learn from interactions over time, improving their responses and recommendations based on user behavior and preferences.
This adaptability makes them increasingly effective as they gather more data.
Features and Capabilities of Virtual Health Assistants
The features of Virtual Health Assistants are diverse and tailored to meet various healthcare needs. One of the primary capabilities is symptom checking, where patients can input their symptoms and receive preliminary assessments or recommendations for further action. This feature can help triage patients effectively, directing them to appropriate care based on urgency.
Another critical capability is medication management. VHAs can remind patients when to take their medications, provide information about dosages, and alert them to potential drug interactions. This function is particularly vital for elderly patients or those managing multiple prescriptions, as it reduces the risk of medication errors and enhances adherence to treatment regimens.
Additionally, VHAs often include features for appointment scheduling and follow-up reminders. By integrating with electronic health record (EHR) systems, these assistants can streamline administrative tasks for both patients and healthcare providers. Patients can easily book appointments or receive notifications about upcoming visits without needing to navigate complex phone systems or wait on hold.
The Role of Virtual Health Assistants in Remote Patient Monitoring
Remote patient monitoring (RPM) has gained traction as a means of delivering healthcare services outside traditional clinical settings. VHAs play a pivotal role in this paradigm shift by enabling continuous data collection from patients’ homes. Through wearable devices or mobile applications, VHAs can track vital signs such as heart rate, blood pressure, and glucose levels, transmitting this information back to healthcare providers in real-time.
This capability allows for timely interventions when abnormalities are detected. For instance, if a patient’s blood pressure readings exceed safe thresholds, the VHA can alert both the patient and their healthcare provider, prompting immediate action. This proactive approach not only enhances patient safety but also reduces hospital readmissions by addressing issues before they escalate into emergencies.
Furthermore, VHAs facilitate communication between patients and providers in RPM scenarios. Patients can easily report changes in their condition or ask questions about their treatment plans through the VHA interface. This ongoing dialogue fosters a collaborative relationship between patients and healthcare teams, ultimately leading to better health outcomes.
Virtual Health Assistants and Chronic Disease Management
Personalized Support for Chronic Conditions
Virtual Health Assistants provide essential support by offering tailored advice based on individual health data. For instance, a VHA designed for diabetes management can analyze a patient’s blood sugar levels and dietary habits to provide personalized meal plans and exercise recommendations. By integrating data from glucose monitors and fitness trackers, the VHA can offer real-time feedback that helps patients make informed choices throughout the day.
Empowering Patients through Education
Moreover, VHAs can facilitate educational resources that empower patients with knowledge about their conditions. By providing access to articles, videos, and interactive tools, these assistants help demystify complex medical information. Patients who understand their conditions are more likely to adhere to treatment plans and engage in self-management strategies that promote long-term health.
Improved Health Outcomes through Virtual Support
This level of personalized care is crucial for maintaining stable health in chronic disease management. By providing ongoing support and guidance, VHAs can help patients better manage their conditions, leading to improved health outcomes and a better quality of life.
The Future of Virtual Health Assistants in Healthcare
The future of Virtual Health Assistants in healthcare appears promising as advancements in technology continue to evolve. With the integration of artificial intelligence becoming more sophisticated, VHAs are expected to become even more intuitive and capable of handling complex medical inquiries. As machine learning algorithms improve, these assistants will be able to provide increasingly accurate diagnoses and treatment recommendations based on vast datasets.
Additionally, the expansion of telehealth services will likely drive further adoption of VHAs in clinical settings. As more healthcare providers recognize the value of remote care solutions, VHAs will play an integral role in enhancing patient experiences and outcomes. The ability to provide immediate support and information will be crucial as healthcare systems adapt to meet the demands of an aging population and rising chronic disease prevalence.
Furthermore, as interoperability between different healthcare systems improves, VHAs will be able to access comprehensive patient records seamlessly. This capability will enable them to deliver more personalized care by considering a patient’s entire medical history rather than isolated data points. The result will be a more holistic approach to patient management that prioritizes individual needs.
Challenges and Limitations of Virtual Health Assistants
Despite their many advantages, Virtual Health Assistants face several challenges that may hinder their widespread adoption in healthcare settings. One significant limitation is the variability in technology literacy among patients. While younger generations may embrace digital health solutions readily, older adults or those with limited technological experience may struggle to navigate VHA interfaces effectively.
Additionally, there are concerns regarding the accuracy of information provided by VHAs. While these systems are designed to deliver reliable responses based on existing data, they are not infallible. Misinterpretations or errors in data processing could lead to incorrect advice or recommendations that may adversely affect patient health outcomes.
Moreover, integrating VHAs into existing healthcare workflows poses logistical challenges for providers. Healthcare organizations must ensure that these digital tools complement rather than disrupt established processes. Training staff on how to utilize VHAs effectively while maintaining high standards of patient care is essential for successful implementation.
Privacy and Security Concerns with Virtual Health Assistants
The use of Virtual Health Assistants raises significant privacy and security concerns that must be addressed proactively. Given that these systems often handle sensitive personal health information (PHI), ensuring data protection is paramount. Healthcare organizations must comply with regulations such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States, which mandates strict guidelines for safeguarding patient data.
Data breaches pose a considerable risk in the digital age; therefore, implementing robust cybersecurity measures is essential for protecting patient information from unauthorized access or exploitation. Encryption protocols, secure authentication methods, and regular security audits are critical components of a comprehensive strategy to mitigate risks associated with VHAs. Furthermore, transparency regarding data usage is vital for building trust between patients and healthcare providers.
Patients should be informed about how their data will be used by VHAs and have control over their information sharing preferences. Establishing clear policies around data ownership and consent will help alleviate concerns surrounding privacy while promoting responsible use of technology in healthcare.
Implementing Virtual Health Assistants in Healthcare Settings
The successful implementation of Virtual Health Assistants within healthcare settings requires careful planning and consideration of various factors. First and foremost, organizations must assess their specific needs and objectives for utilizing VHAs. Identifying target populations—such as patients with chronic conditions or those seeking preventive care—can help tailor the VHA’s functionalities accordingly.
Training staff members on how to effectively integrate VHAs into their workflows is another critical step in implementation. Healthcare professionals should understand how these digital tools complement traditional care methods rather than replace them entirely. Providing ongoing support and resources will ensure that staff feel confident using VHAs as part of their practice.
Additionally, engaging patients during the implementation process is essential for fostering acceptance and utilization of VHAs. Gathering feedback from patients about their experiences with these tools can inform future enhancements while ensuring that the technology meets their needs effectively.
Case Studies and Success Stories of Virtual Health Assistants in Patient Monitoring
Numerous case studies highlight the successful application of Virtual Health Assistants in patient monitoring across various healthcare settings. One notable example is the use of a VHA by a large hospital system that implemented an AI-driven chatbot for post-operative care follow-up. Patients were able to report symptoms directly through the chatbot interface, which triaged responses based on severity before alerting clinical staff when necessary.
This approach significantly reduced unnecessary emergency room visits while ensuring timely interventions for those who required additional care. Another success story comes from a diabetes management program that integrated a VHA into its services. Patients using this assistant received personalized meal plans based on their glucose readings while also being reminded about medication schedules through push notifications on their smartphones.
The program reported improved adherence rates among participants as well as better overall glycemic control compared to traditional management methods. These examples illustrate how Virtual Health Assistants can enhance patient monitoring by providing timely support while empowering individuals to take charge of their health journeys effectively. As technology continues to advance, it is likely that more innovative applications will emerge within this domain, further transforming how healthcare is delivered.